АФФЕКТИВНОЕ НАРУШЕНИЕ У ЛЮДЕЙ С БОЛЕЗНЬЮ АЛЬЦГЕЙМЕРА И СОСУДИСТОЙ ДЕМЕНЦИЕЙ
Научная статья
Крстеска Р. *
ORCID: 0000-0002-1273-1842,
Психиатрическая больница “Скопье”, Cкопье, Македония
* Корреспондирующий автор (r_krsteska[at]yahoo.com)
Аннотация
Введение: оценка и лечение аффективных симптомов у людей с деменцией играют важную роль в их вовлечении в повседневную деятельность, взаимоотношения и качество жизни как их самих, так и их семей.
Цель: Наша цель состояла в оценке аффективных нарушений у людей с болезнью Альцгеймера (БА) и сосудистой деменцией (СД).
Предмет исследования и метод: Мы оценивали больных по шкале аффективных нарушений BEHAVE-AD (30 человек с БА и 30 с СД), присваивая им от 0 до 3 баллов в зависимости от степени выраженности симптомов.
Результаты: Аффективное нарушение было обнаружено у 86% людей с сосудистой деменцией и у 36,6% у людей с болезнью Альцгеймера.
Вывод: Понимание природы изменений настроения у людей с БА может помочь в планировании надлежащего фармакологического и нефармакологического лечения, а также в предоставлении соответствующих рекомендаций лицам, осуществляющим уход за ними.
Ключевые слова: болезнь Альцгеймера, сосудистая деменция, аффективные расстройства.
THE AFFECTIVE DISTURBANCE IN PEOPLE WITH ALZHEIMER’ AND VASCULAR DEMENTIA
Research article
Krsteska R. *
ORCID: 0000-0002-1273-1842,
Psychiatric hospital “Skopje”, Skopje, Macedonia
* Corresponding author (r_krsteska[at]yahoo.com)
Abstract
Introduction: The evaluation and treatment of affective symptoms in the people with dementia have an important role in the engagement in daily activities, relationships and the quality of life for them and their families.
Objective: Our aim was to evaluate Affective Disturbance in people with Alzheimer’s (AD) and vascular dementia (VD).
Subjects and Methods: We assessed the scores of the Affective Disturbance Subscale of the BEHAVE-AD in 30 people with AD and 30 people with VD, scoring 0-3 based on severity rating of the symptoms.
Results: The Affective Disturbance was present in 86% of people with vascular dementia and in 36.6% in people with Alzheimer’s dementia.
Conclusion: An understanding of mood symptoms in people with AD can aid in planning appropriate pharmacological and nonpharmacological treatment and also to help in giving appropriate advice to caregivers.
Keywords: Alzheimer’s desease, vascular dementia, Affective Disturbance.
Introduction
In many developing countries studies for dementia are missing. The specialists are meeting patients in moderate and severe stages of dementia. Alzheimer disease and other degenerative and vascular dementias can be associated with affective symptoms that are part of the Behavioral and psychological symptoms of dementia (BPSD). BPSD are a source of distress and burden for family and professional caregivers, and are also associated with more rapid institutionalization and increased morbidity and mortality for people with AD [1]. Severe or chronic diseases associated with high rates of depression include stroke (30 to 60%), Parkinson’s disease (40%), Alzheimer’s disease (20 to 40%), and dementia (17 to 31%) [2]. Shah et al. [3] said that BPSD have been poorly studied in developing countries, in ethnic minority groups in a given country and in cross-national studies. Often is difficult to diagnose depression in elderly patients with dementias. In the literature is reported a wide variation of the percentage representation of individual symptoms of BPSD [4], [5].
Brodaty et al. [6] in nursing home residents with the BEHAVE-AD scale found that over 90% of clients showed at least one behavioral disorder, psychoses in 60%, depression at 42%, and disruption of the activities or aggression at 82%.
Most studies confirm that depression is more common and difficult in the people with vascular dementia than Alzheimer’s dementia [7], [8], [9]. In our country the patient’s family bears the huge burden because of dementia and the presence of the BPSD are complicate highly the state of patient and his family, as well as of the caregivers in institutions who care for these people.
In several studies the syndromic nature of each of the 7 categories of symptoms assessed with the BEHAVE-AD, were ivestigated in regard to the pharmacological intervention.
Objective
The aim of this research work is to analyse the depressive symptoms of patients with Alzheimer’s and vascular dementia.
Subjects and Methods
The study included 30 patients with Alzheimer’s dementia and 30 patients with vascular dementia. All patients fulfilled the ICD-10 (International Classification of Mental and Behavioral Disorders) criteria for Alzheimer’s or vascular dementia.
In our investigation we used: clinical interview, direct observation, proxy report and the Affective Disturbance Subscale of the Behavioral Pathology in Alzheimer’s disease Rating Scale (BEHAVE-AD published in 1987) [10]. The scale separates cognitive and functional symptoms that occur in AD from behavioral disturbance symptoms. The BEHAVE-AD symptoms in the scale constitute 7 individual BEHAVE-AD symptomatic categories of AD [1].
Results with discussion
In our study depressive symptoms were present in the people with vascular and Alzheimer’s dementia (86% vs. 36.6%). A higher percentage was found in the group of patients with VD than in group with AD (Fig. 1). The division of the scores of the Affective Disturbance Subscale scored 0-3 based on severity (severally, moderately, mildly, not at all) in the group with Alzheimer’s disease was: moderately 23.3%, mildly 13.3% and not at all 63.4% vs. moderately 83.3%, mildly 3.3% and not at all 13.4% in the group with vascular dementia (Fig. 1).
In our sample, the percentage of depressive symptoms in people with Alzheimer’s dementia was 36.6% which is in agreement with the other authors who find depression in Alzheimer’s dementia in 35-50%, and in the group with vascular dementia it was present in 86.6% [11].
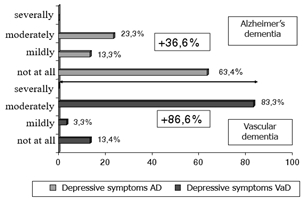
Fig. 1 – The division of the scores of the Affective Disturbance Subscale (depressive symptoms) scored 0-3 based on severity
Several studies reported different degrees of depression in dementia, Purandare N et al. [12] said there were studies who refer to depression among people with dementia between 1.5 and 28%, while referring to depressive symptoms of the percentage were higher, between 0-87 percent.
The mean value of the total score of the Affective Disturbance Subscale of BEHAVE-AD in the group with vascular dementia was 4.7 and in the Alzheimer’s dementia group 1.43. The difference between the mean values in the two examined groups is statistically significant for p = 0.0000 (Table 1.).
Table 1 – The mean score of the Affective Disturbance Subscale of BEHAVE-AD
| Group with Dementia | x | ±SD | minimum |
| Vascular dementia | 4.7 | 2.05 | 0 |
| Alzheimer’s dementia | 1.43 | 2.04 | 0 |
Note:*p = 0,0000
Our data are in line with the literature data about the depression with greater representation and difficulties in vascular dementia than Alzheimer’s dementia [7], [8], [9]. O’Brien [11] in his study on behavioral symptoms noted that there is a particularly strong relationship between cerebrovascular disease and depression.
The qualitative analysis of the depressive symptoms in our study in the two groups of respondents shows that the symptoms often fluctuate, the symptoms are irregular, are associated with psychotic symptoms and other neuropsychiatric and behavioral symptoms, and caregivers do not emphasize them as the main symptom that were problem for them or a motive for examination or hospitalization. Pang et al. [13] came to similar findings in their study in the families of patients with Alzheimer’s dementia among Americans and Chinese in Taipei and Hong Kong and were surprised by the results that, these symptoms of the family showed a similar relationship, while the Chinese families were less affected by depression than the American family.
With our research we associate ourselves with the view of several authors in the literature that certain, categorical diagnostic criteria and approaches can be difficult to apply, and lacking diagnostic criteria specific to depression in dementia [14], [12].
The syndromic nature of the 7 BEHAVE-AD symptomatic categories with respect to the pharmacological treatment intervention was also observed by several authors [15]. Reisberg et al. [1] emphasized the importance of distinguishing BPSD and the need for an appropriate assessment methodology. They talked about the importance of providing a framework for further progress in the treatment of BPSD in people with AD and, consequently, continuous improvements in the lives of individuals with AD and those who share the burden of disease with them. They discussed the kinds of medications that alleviate behavioral symptoms on these measures as well as the problems and possibilities for further advances with these medications.
Conclusion
Our study gives a small contribution to clarify the presence of depressive symptoms in people with dementia. More studies are needed for this topic in developing countries. The results of our study have shown the presence of depressive symptoms in people with dementia in our population. Our findings suggest that an understanding of depression in people with dementia can aid the treating physician in giving appropriate advice to caregivers and also help them in planning appropriate pharmacological and nonpharmacological treatment. Epidemiological studies and education of healthcare providers for dementia and BPSD is needed. The syndromic nature of the 7 BEHAVE-AD symptomatic categories are important for further progress in the treatment of BPSD in people with AD and other dementia.
| Конфликт интересов
Не указан. |
Conflict of Interest
None declared. |
Список литературы / References
- Reisberg B. The BEHAVE-AD Assessment System: A Perspective / Reisberg B., Monteiro I., Torossian C. and others. A Commentary on New Findings, and A Historical Review. Dement Geriatr Cogn Disord. 2014; 38(1-2): 89–146.
- Finkel S. Introduction, Clinical and research update: new findings. International Psychogeriatrics / Finkel S. 2000; 12(1); 9-12.
- Shah A. Behavioural and psychological signs and symptoms of dementia across cultures: current status and the future / Shah A., Dalvi M., Thompson T. Int J Geriatr Psychiatry. 2005; 20(12):1187-95.
- Wasiak B. Frequency and Intensity of Behavioral and Psychological Symptoms in the Course of Alzheimer’s Disease / Wasiak B., Gabryelewicz T., Luczywek E. and others. Psychiatr Pol. 2001;35(1):93-107.
- Lam L.C. Behavioral profile of Alzheimer’s disease in Chinese elderly-a validation study of the Chinese version of the Alzheimer’s disease behavioral pathology rating scale / Lam L.C., Tang W.K., Leung V. and others. Int J Geriatr Psychiatry. 2001; 16(4):368-73.
- Brodaty H. Psychosis, depression and behavioural disturbances in Sydney nursing home residents: prevalence and predictors / Brodaty H., Draper B., Saab D. and others. Int J Geriatr Psychiatry. 2001; 16(5):504-12.
- Lyketsos C.G. Mental and behavioral disturbances in dementia: findings from the Cache County study on memory in aging / Lyketsos C.G., Steinberg M., Tschanz JT.and others. Am J. 2000; 157 (5): 708-14.
- Cummings J.L. Neuropsychiatric aspects of multiinfarct dementia and dementia of the Alzheimer’s type / Cummings J.L., Miller B., Hill M.A. and others. Arch Neurol.1987; 44:389-93.
- Sultzer D.L. A comparation of psychiatric symptoms in vascular dementia and Alzheimer’s disease / Sultzer D.L., Levin H.S., Mahler M.E. and others. Am J Psychiatry. 1993; 150:1806-12.
- Reisberg B. Behavioral symptoms in Alzheimer’s disease: phenomenology and treatment / Reisberg B., Borenstein J., Salob SP. and others. J Clin Psychiatry. 1987;48(5):9–15.
- O’Brien J. Behavioral symptoms in vascular cognitive impairment and vascular dementia / O’Brien J. Int Psychogeriatr. 2003; 15 (1):133-8.
- Purandare N. Depressive symptoms in patients with Alzheimer’ disease / Purandare N., Burns A., Craig S. and others. Int J Geriatr Psychiatry. 2001;16: 960–964.
- Pang F.C. Effect of neuropsychiatric symptoms of Alzheimer’s disease on Chinese and American caregivers / Pang F.C., Chow T.W., Cummings J.L. and others. Int J Geriatr Psychiatry. 2002; 17(1):29-34.
- Frans R. Phenomenology of Depression in Dementia / Frans R., Verney J, Visser PJ. International Psychogeriatrics.2000;12 (1):129-134.
- Levy M.A. A trial of buspirone for the control of disruptive behaviors in community-dwelling patients with dementia / Levy M.A., Burgio L.D., Sweet R. And others. Int J Geriatr Psychiatry. 1994;9:841–848.






